Date: 04/2009 
One Fish, Two Fish, Red Fish, Blue Fish
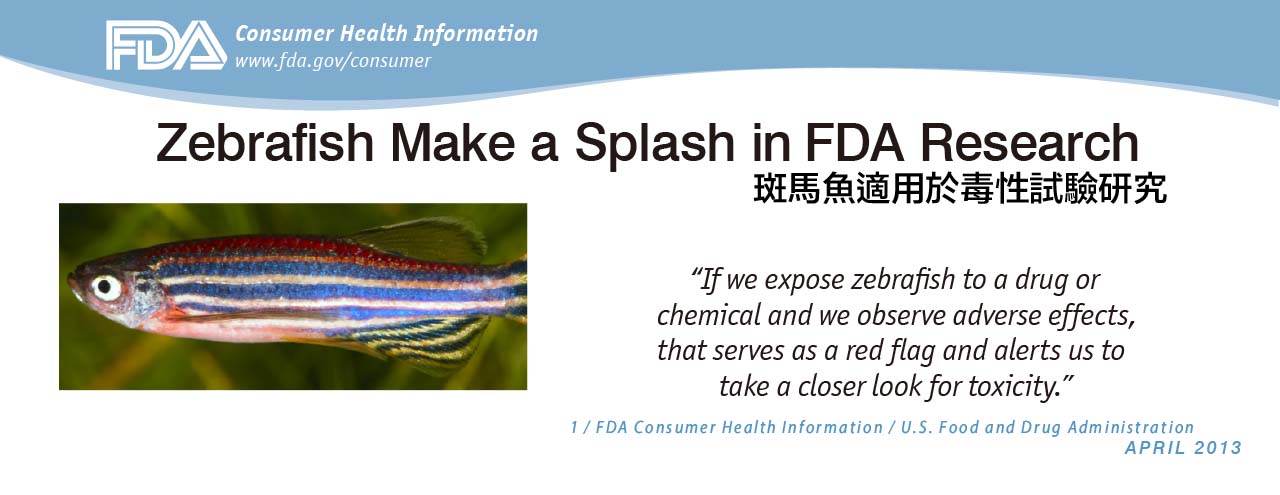
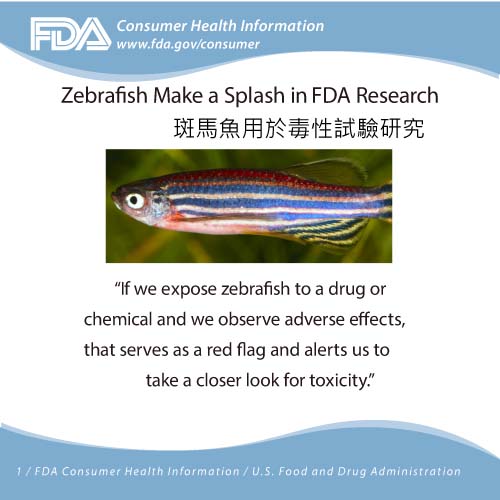
To all appearances, the zebrafish is your typical aquarium dweller. But over the past 30 years, the tiny translucent creature has become an important research model used by scientists to study a host of conditions, including cancers, neurological diseases and blood disorders. As a result, today you’re as likely to find zebrafish inhabiting laboratories of biomedical research centers as you are to find them in pet stores or home fish tanks.
Studying Blood Disorders
Zebrafish measure less than two inches long and weigh less than an ounce. Yet in terms of organ development, they are genetically similar to humans, making them an ideal model to use in studying various types of anemia and other blood diseases, as well as in understanding how the body regenerates tissues that have been damaged by disease or trauma. 
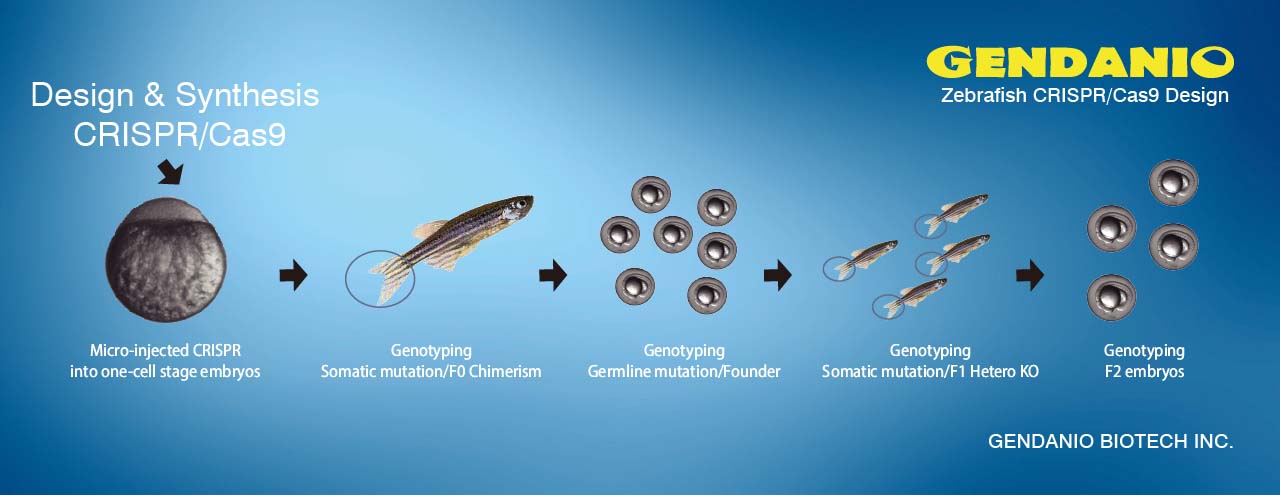
“Studying the development of zebrafish embryos enables us to identify genes and chemical agents that affect iron metabolism and other processes,” explains Fraenkel. “The zebrafish provides an excellent system for the identification and analysis of genes involved in iron metabolism and erythroid (red blood cell) development. In this way, we have been able to conduct large-scale ‘screens’ that are providing us with insights into hereditary and acquired iron overload syndromes, which can result in failure of the liver, heart and pancreas.” 
In the March 19 cover story in the journal Blood, Fraenkel and her coauthors describe their discovery of the molecular underpinnings responsible for the regulation of iron absorption and utilization, using the zebrafish embryo as a model.
Using Zebrafish to Learn About Stem Cells
North’s research uses zebrafish as a screening tool to identify regulatory pathways that can control the formation of blood stem cells -- which in turn develop into each of the body’s various blood cell types. In earlier work, North and her colleagues identified several compounds that increase the production of blood-forming, or hematopoetic, stem cells.
“We knew that these compounds could be of clinical importance to enhance the success of bone marrow or cord-blood transplantation,” says North, explaining that one of the goals of hematopoetic stem cell transplantation is to restore the immune systems of patients whose blood cells have been depleted by cancer therapy.
In a study published March 20 in the journal Cell, North showed that the same molecules that interact to shape embryonic development also play a role in adult tissue regeneration. “It’s been very exciting,” says North, explaining that their initial analysis uncovered a novel role for the prostaglandin E2 molecule, a naturally occurring inflammatory mediator, which plays a central role in stem cell formation.
Her recent work, conducted in collaboration with Wolfram Goessling, PhD, of Brigham and Women’s Hospital, extends those previous observations to show that PGE2 directly influences the WNT signaling pathway, known to be a central regulator of cell proliferation. The scientists additionally found that this interaction is not specific to blood cells.
“We think we have uncovered a general mechanism that the body uses to respond to injury,” says North, adding that a stabilized version of PGE2 was recently approved by the U.S. Food and Drug Administration for investigational clinical use in the setting of cord blood stem cell transplantation for the treatment of leukemia. “This marks the first example of taking a small molecule isolated from a screen in zebrafish and bringing it into the clinic,” she adds.
Source: BIDMC